BBC News, Toronto
 Canadian Press
Canadian PressMorgan Birch’s four-month-old daughter Kimie suddenly became confused when she fell ill with a fever and a rash.
At first, Alberta mothers thought it was a common side effect of immunization, or a case of chicken pox. Ms. Birch then consulted her 78-year-old grandmother, and her mother immediately realized Kimie’s illness.
“That’s measles,” said her grandmother. Ms. Birch was stunned because she thought the disease had been eradicated.
A lab test later confirmed her grandmother’s hypothesis: Kimmy had measles, which may contract after a routine visit to an Edmonton-area hospital a few weeks ago.
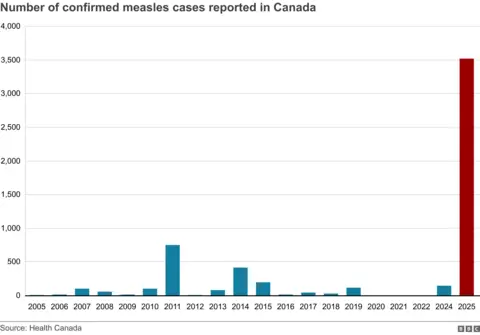
Kimie is one More than 3,800 people in Canada have contracted measles In 2025, most are children and babies. This number compares Number of confirmed U.S. casesAlthough Canada is much smaller.
Now, Canada is the only Western country to list the top ten measles outbreaks. According to CDC dataranked eighth. Alberta is the epicenter of the current outbreak, with the highest per capita measles dispersion rate in North America.
The data raises questions about why the virus spreads faster in Canada than the United States and whether Canadian health authorities are doing enough to contain the virus.
In the United States, the rise of measles is partially linked to public figures like Health Secretary Robert F Kennedy Jr, although he has since recognized that the measles vaccine is safe.
However, Maxwell Smith, a descendant of the Public Health Society of Canada at Western Ontario University, noted that Canada does not have outstanding RFK JR-like numbers in public health.
“I think there are other things to be interrogated,” Dr. Smith said. “Looking at the Canadian context adds another layer of complexity to that.”
In North America, Europe and the UK, measles are generally increasing. The U.S. case has reached a 33-year high this year. Although England reported nearly 3,000 confirmed infections in 2024This is the highest count since 2012.
Canada’s 2025 figures exceed these two figures. The country has not seen so many cases of measles since the disease was announced to be eliminated in 1998. This year, the last peak was in 2011, with about 750 cases reported.
The MMR vaccine is the most effective way to fight measles, a highly contagious and dangerous virus that can cause pneumonia, brain swelling and death. Jab is 97% effective and can also be immune to mumps and rubella.
 Morgan Birch
Morgan BirchHow measles spread in Canada
The provinces that are most affected are Ontario and Alberta, followed by Manitoba.
Health authorities in Ontario said the outbreak began in late 2024 when a man contracted measles at a large Mennonite party in New Brunswick and returned home.
The Mennonites are a Christian group rooted in Germany and the Netherlands in the 16th century and have since settled in other parts of the world, including Canada, Mexico and the United States.
Some modern modern lifestyles, while conservative groups lead simpler lives, limit the use of technology and rely only on modern medicine when necessary.
In Ontario, the disease mainly spreads to the bass Mennonite community in the province’s southwestern language, with vaccination rates historically low due to some members’ religious or cultural beliefs about immunization.
According to Ontario Public Health data, almost all infected people are not vaccinated.
Catalina Friesen, a healthcare worker at a mobile clinic, who serves the Mennonite population near Aylmer, Ontario, said she first realized the outbreak in February when a woman and a five-year-old had an ear infection. It turned out to be a symptom of measles.
“This is the first time I’ve seen measles,” Ms Friesen told the BBC.
Since then, cases have spread rapidly, and by late April, Ontario has had more than 200 peaks per week.
Despite the sharp drop in newly confirmed cases in Ontario, Alberta has become the next hot spot. There, the difference happened so quickly that health officials could not accurately point out the way or where the outbreak occurred, Dr. Vivien Suttorp, a health care officer in southern Alberta.
She also said that in her 18 years of public health, she has not seen any outbreaks.
Ms. Friesen pointed out that Canada’s low conservativeness is higher than that of the United States, which may be a factor in the higher number of cases.
But the Mennonites are not a boulder, and many have been vaccinated, she said. What changed was the rapid spread of misinformation against vaccines in her community and coalition after the 19th pandemic.
“There are rumors that immunity is harmful to you,” Ms. Friesen said.
This amplifies the general distrust of the healthcare system, she said, historically excluding it from her community.
“Sometimes we are sometimes overwhelmed or looked down upon because of our background,” she said, adding that she herself experienced discrimination in hospitals based on the assumptions of her beliefs.
Vaccine hesitation
Experts say it is difficult to point out why measles is bigger in Canada than the United States, but many agree that cases in both countries may be underestimated.
“Our numbers in Alberta are just the tip of the iceberg,” Dr. Satop said.
But there is a big reason that drives the outbreak: low vaccination rates, said Janna Shapiro, a postdoctoral researcher at the University of Toronto’s Center for Preventable Diseases.
Dr Shapiro said there was an “opportunity element” at work, accidentally introducing the virus into a community and spreading among those without protection.
“The only thing that will stop the outbreak is to increase the vaccination rate,” she said. “If the public is unwilling to get the vaccine, it will continue until the virus can no longer find an acceptable host.”
Overall, research shows that vaccine hesitation in Canada has risen since the pandemic, and the data reflects that. In southern Alberta, for example, the number of MMR vaccines administered fell by nearly half from 2019 to 2024.
The authorization of the Covid-19-19 vaccine has been met with strong opposition from some during the pandemic, prompting Ottawa’s so-called “freedom fleet” protests to lock truckers in the city for two weeks in 2021.
Dr. Shapiro said the opposition has expanded to other vaccines.
The disruption related to the pandemic has also led to routine immunizations from some children. Dr. Shapiro said that with measles being greatly eliminated, families may not prioritize vaccination for children.
That was not the case for Ms. Birch, who started routine immunization of her baby Kimie once she was eligible. But Kimie is still too young for the measles vaccine, usually in Alberta for 12 months.
Dr Saltop said Alberta has lowered its age cap since then to cope with the recent outbreak, with more people receiving the vaccine.
Health departments across the country are also trying to encourage people to get vaccinated through announcements and broadcast ads. But during the 199 pandemic, the reaction was softer than that, health officials said.
Ms Birch said Kimie has recovered slowly since then, although she continues to monitor the long-term effects of the virus.
The Alberta mother said she felt sad and fearful when she learned her daughter had measles, but was also “frustrated and upset” with those who chose not to vaccinate their children.
She called on people to pay attention to public health guidelines and “protect those who cannot protect themselves.”
Ms. Birch said: “My four-month-old shouldn’t have measles in 2025.”

Health & Wellness Contributor
A wellness enthusiast and certified nutrition advisor, Meera covers everything from healthy living tips to medical breakthroughs. Her articles aim to inform and inspire readers to live better every day.





